Run Like a Mother: Your Guide to Running in Pregnancy and Postpartum
This one goes out to all my mother runners out there.
I’m the first to admit that I am NOT a runner. It isn’t a form of exercise I like at all, but I have had many clients who do love running. In fact, I talk to women every day who ran throughout their pregnancies and picked it back up as early as possible postpartum. Most women are told that if they did it before pregnancy, it’s safe to do throughout pregnancy. In the postpartum period, women are often given the “all clear” at 6-weeks with no instruction on HOW to do that. So, it ends up being a situation where they just go back to what they did before.
Running is a super easy thing to do. You just lace up your shoes and go outside. No gym membership, no list of exercises, a dose of fresh air, often you can take your baby or toddler in a stroller. And if you actually enjoy running, it can be a huge stress-reliever and an amazing way to boost your mood.
By no means am I saying running is bad in pregnancy and postpartum. I am saying that running may not be the best thing for a birthing person in their third trimester or in the early months postpartum. It may not be the best thing for that person *right now*, even in earlier pregnancy or later postpartum.
I am saying that we need to look at the bigger picture. This blog aims to do just that. First we’ll look at why running may not be the best choice in pregnancy and early postpartum from a pressure standpoint, then we’ll dive into considerations to make and alternate exercise choices for pregnancy, then lastly we’ll chat about how and when-ish to get back into running postpartum.
You ready for this? It’s gonna be a good one.
Under Pressure
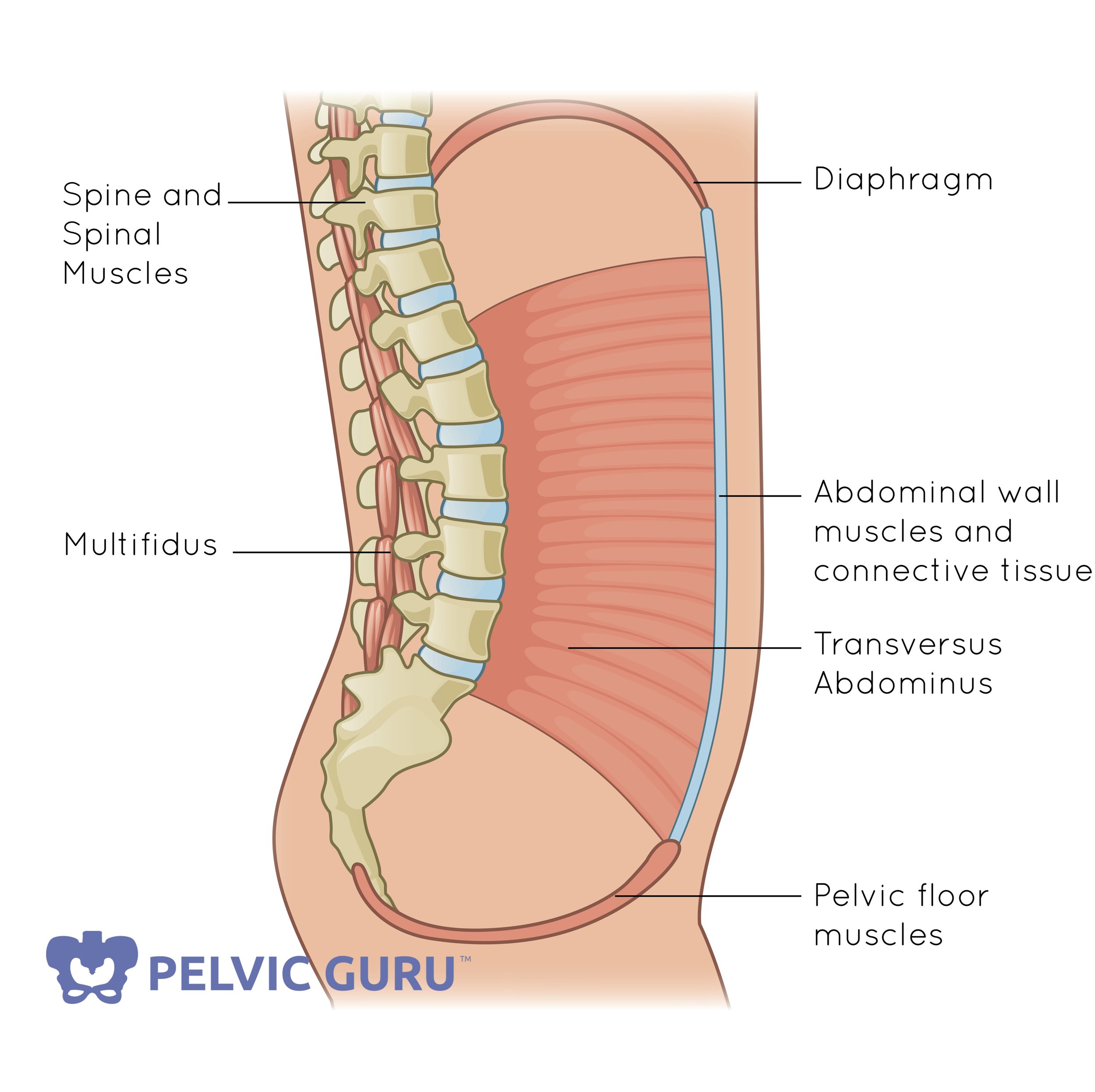
Pelvic Guru owns the rights to this image.
The core canister- which is made up of the deep abdominals at the front, diaphragm at top, and pelvic floor on the bottom- is one big pressure system. As we inhale the pressure increases causing the core to expand and the pelvic floor to drop down and ideally relax. When we exhale, the pressure decreases and the core/pelvic floor contract. It kind of creates this undulation wave-type movement is really cool to watch.
Now, what we’re concerned about in this particular blog is what’s happening to the pressure system during pregnancy and how those changes impact the body post-birth.
When we stand, sit, or basically do anything upright there’s some pressure placed on the pelvic floor… hi there, gravity! When we do dynamic exercises like jumping or running, that causes more downward pressure on the pelvic floor. And while a jump may be a one or ten times thing, running is repetitive and also requires you to load a single leg during that impact. Each time the foot hits the ground, pressure increases down.
Before we move on… This is NOTHING to freak out about and is exactly WHY our pelvic floors are there, to shoulder that load and create a little trampoline for our organs. It’s pretty rad, but also something we need to take into consideration when the pressure system is already altered or if someone is experiencing symptoms like leaking or pain.
Image Copyright Mom365
During pregnancy, the core canister changes. As the uterus expands to house an entire human person, the abdominals expand, the lungs are pushed up, and there’s more pressure down on the pelvic floor. The reason running may not be the best exercise choice in pregnancy is because you’re placing more pressure on an already stressed system.
In the postpartum period, your body is recovering from a HUGE event. The placenta left a dinner plate-sized wound in your uterus that is healing, you’re likely exhausted, up feeding a baby at all hours, wearing the same yoga pants for the 10th day in a row… Again we’re adding more pressure to an already stressed system.
Now you may be asking, “But Madison, what if I had a C-section? My pelvic floor is fine, right?”
I once did an experiment for social media where I placed a bowling ball in a box for a few days. The bowling ball represented roughly the weight of the baby, placenta, and amniotic fluid. The box was a poor representation of a pelvic floor, the real thing is MUCH more dynamic.
When I took the ball out, the box was misshapen. The weight of the ball put pressure on the box and changed its structure. And when I picked up the box, it wasn’t as strong as when I put the bowling ball in it… mainly because I left it out in the rain but I found that a fairly accurate representation of 9 (10) months of pregnancy.
Here’s my point, even though I didn’t push the ball through the bottom of the box to get it out, it still had that pressure and the changes that occurred because of it.
How you birthed plays a part in pelvic floor health post-birth for sure, but having a C-section doesn’t exclude you from possible pelvic floor related issues, exercise considerations, or rehab!
Growing a baby naturally increases pressure in the core canister and as pregnancy progresses, the way we breathe and move can change. These movement and breathing patterns we adopt in pregnancy can stick around and leave the body feeling really uncoordinated. These things are important to take into consideration when assessing risk versus benefit of impact exercises during pregnancy and early postpartum and a great way to ensure you’re setting yourself up for long term pelvic health and symptom-free activity.
Which leads me right into the how. HOW do we make these considerations and when? What are some alternate exercises to running and when should we choose them? I’ve got your back.
Pregnancy Running Considerations
In the first trimester we’re dealing with HORMONAL considerations. Fatigue, nausea, changes in mood, how the body is feeling, low energy. These are all things that should be taken into consideration, not necessarily from a pressure standpoint- though many women who have experienced symptoms, like leaking, in the past note increased symptoms in the first trimester- but from a more physical and mental comfort one. This may not be the time to push yourself to run a marathon if you’re feeling tired or sick, but a run around the neighborhood could help boost mood and is likely fine for your body.
In the second trimester we’re dealing with lots of PHYSICAL changes. The second trimester can usually mark a time where energy is high and you’re feeling really good. Getting up and moving can be really great for the body, but you may notice the need to make changes in your activity from a physical standpoint. This may happen earlier for second time moms or moms with different body shapes and torso sizes. As the baby grows, steady state running may need to be replaced with short distance running mixed with walking phases. The mix-it-up variation allows the pelvic floor a break by taking some of that impact pressure off while still getting a good sweat on. Strength training to support single leg loading patterns and glute/hip strength can be really beneficial for runners, especially those in pregnancy.
In the third trimester we’re dealing with all kinds of changes in a body that is hormonally and physically preparing for birth. This trimester is a time that many birthers experience pelvic pain, back pain, and other aches and pains- though I talk to moms every day who start seeing these things as early as the second trimester. These things should be taken into consideration when discussing running postpartum. It isn’t necessary to run or workout through pain. Running in the third trimester is an “it depends” kind of thing. Some women run and are fine in the third trimester, some are not. In either case, pelvic floor consideration-wise, the pressure system of the core canister is completely changed at this point. You’ve got the lungs and organs pushed up and a little one (or ones) using your bladder as a punching bag. I’d be more inclined to explore other options and suggest activities like hill walking, sled (or stroller) pushes, and strength training. Not forever, just for now.
Running isn’t bad to do in pregnancy. However, as pregnancy progresses running may not be right for your body *right now*. Strategies like intervals, mixed terrains, and hill walking can keep the love for running alive while also reducing pressure on the pelvic floor. Not only are these great ways to modify your running practice during pregnancy, they are also helpful tools in your return to running postpartum!
Running Considerations Postpartum
Many women are being cleared for all activity at 6-weeks without a referral to a pelvic floor physical therapist or any guidance on HOW to return to exercise after having a baby. I’ve spoken to women who are back out running as early as 3 weeks postpartum.
When the baby comes out, all the changes that happened don’t just go away. The pressure placed on the pelvic floor and core during that time of baby growing can cause many people to shift their patterns of breathing and moving. Postpartum is a time where your body is trying to figure out how to coordinate itself again.
Not only that, it’s also a time where you’re getting very little sleep, figuring out life with a newborn, and constantly at the beck and call of someone else.
Things like how you birthed, what your birth experience looked like, how you’re recovering, if you birthed vaginally or via C-section, what labor was like, if there was any tearing, sleep, stress, and if you’re experiencing depression or anxiety are super important to consider when returning to exercise postpartum.
First and foremost, everyone should see a pelvic floor physical therapist post-birth if they have the means and access to one. A good PFPT can help you heal better from birth, get you started with scar massage (C-section and perineal), and give you more guidance than “you’re cleared”.
In the early postpartum period, running might feel like the easiest thing you can do. No fuss, no stress. Just take the stroller out and go. I highly suggest a return to running be very gradual, beginning with walking and a goal-specific strength training routine. This will help build endurance in the pelvic floor and strength in the muscles needed to support running.
For example, single leg loading and hip strength are two important things in running. A few exercises I might suggest to someone wanting to return to running are below:
Level 1- Split Squat
Level 2- Step Up with Eccentric Lower
Level 3- Single Leg Deadlift to Lunge
Once we’ve mastered these exercises, moving on to more impact type ones, like single leg hops, are beneficial to assess any symptoms running may bring on. As strength increases, walks turn into hill walks, then short bouts of jogging mixed with walking, gradually increasing time of jogging and running bouts as the body is ready.
Taking it slow can set you up for crushing your long term running goals, whatever they may be. After all, you wouldn’t go bang out a marathon without training for it first- right?
Remember, slow IS fast.
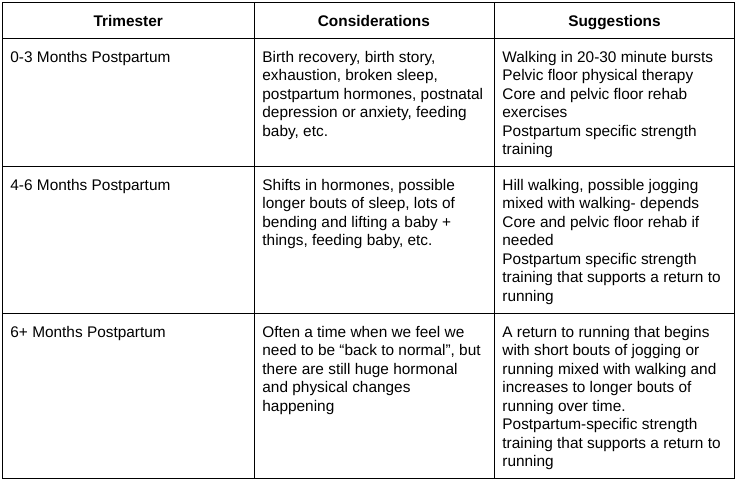
In the above table, I’ve given a rough timeline for a return to running postpartum but every single person is different. Having a pelvic floor physical therapist and a coach trained in working with postpartum populations can give you more individual guidance and get you back to the activities you love faster.
My goal is to never dissuade anyone from activity because research shows us how beneficial it is, and of course, it’s what I do as a coach. I do, however, want to help set parents up for long-term pelvic health by offering suggestions that fit their body at every stage and phase of parenthood. Running is an activity that *can* be great in pregnancy, but one that does put more pressure on a body that is changing tremendously. How the body changes in pregnancy is a big consideration when determining if running is right for your body, during this time we want to do exercise in a way that supports your body and the changes its going through. In the postpartum period, the goal is to heal the body well with a gradual return to higher impact activity to set you up for long term pelvic health and fitness success.
Was this information on running in pregnancy and postpartum helpful? If so, share with your friends!