Pelvic Organ Prolapse and Pregnancy- My Top Three Tips at Navigating POP Through Pregnancy and Birth
A pelvic organ prolapse diagnosis can often be disheartening, especially when you aren’t sure you’re done having kids. When going into another pregnancy and birth, there can be a lot of questions about managing your pelvic organ prolapse during the entire pregnancy and fears about making it worse where birthing is concerned. As a trainer who works with women who have pelvic floor dysfunction like pelvic organ prolapse and a birth doula, some of the questions I get are:
“Will pregnancy make my POP worse?”
“What birth positions will be protective of the pelvic floor and which ones will make it worse?”
“Should I choose a C-section rather than a vaginal delivery?”
While there is no tried and true way to know what may happen during pregnancy and birth, there are ways to manage pelvic floor symptoms during pregnancy and going into birth to help you feel less fear about the outcome. In this blog, I’ll talk about how to manage your pelvic floor symptoms during pregnancy and give you some tips on birth as well- know that HOW you birth is ultimately your choice.
What is Pelvic Organ Prolapse?
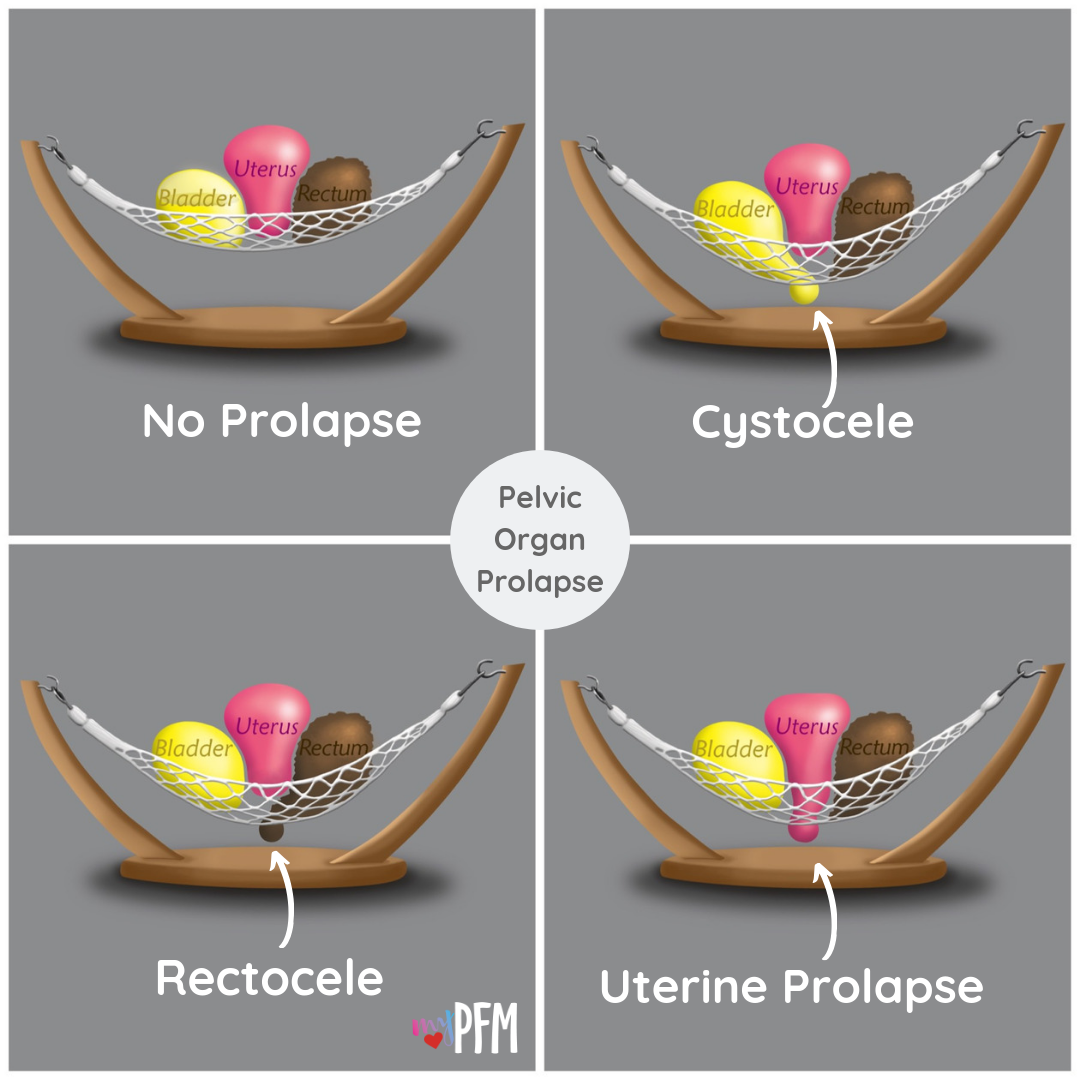
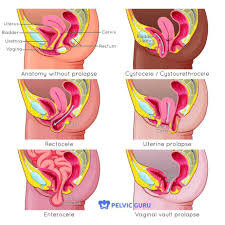
Pelvic organ prolapse is when the pelvic organs descend down and into the vaginal canal. There are three types: bladder, uterine, and rectal. Some symptoms of pelvic organ prolapse include: dragging or heaviness feeling in the vagina- especially after long bouts of standing or walking, bulging or tampon falling out sensation, urinary incontinence, fecal incontinence, and trouble emptying your bladder or bowels.
Though pelvic organ prolapse is not often talked about, newer research shows that UP TO 4 IN 10 WOMEN HAVE PELVIC ORGAN PROLAPSE DURING THEIR LIFE.
Stages of Pelvic Organ Prolapse
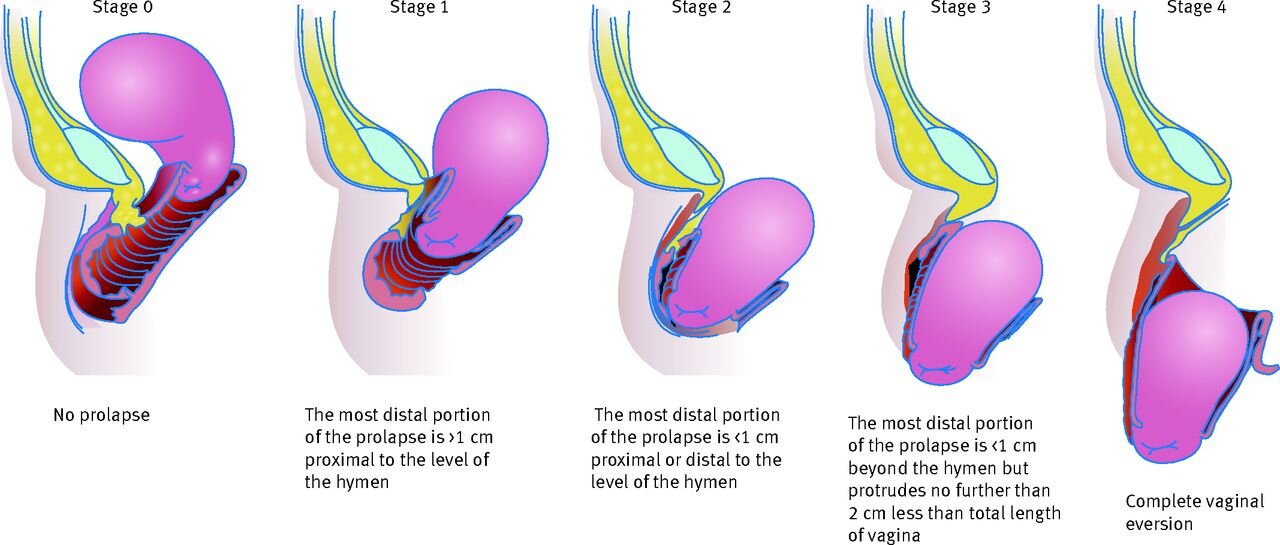
There are 4 grades of prolapse ranging from a 0-4. Zero degree basically means the organs are in their "normal" position. The rest of the degrees depend on how far into the vagina the organ(s) descend. Here's one thing this photo doesn't tell you- a person with a first degree prolapse could be highly symptomatic while another person who has a second degree prolapse may not be experiencing any symptoms and may not even know they have prolapse. It is highly variable and there is no one size fits all.
Newer studies are even showing nulliparous women (women who haven’t had babies) who are sexually active have some descent of the pelvic organs, which may indicate that a zero to low grade first degree may be the “norm” for pelvic organ descent.
Often women are terrified they won't be able to do anything after a POP diagnosis, but that simply isn't true. There are exercises and strategies that can help you manage your symptoms and even reduce the grade of prolapse with the help of a pelvic floor physical therapist.
How to Manage Pelvic Organ Prolapse During Pregnancy
Let me start by saying that every body is completely different, as I always say. What works for one individual may not work so well for another, so the next two points stem from that fact. Suggestions would also depend on severity or type of symptoms and history of that specific person. This article is here to give you a general outline, not to diagnose or treat individuals and is not intended as medical advice. Always seek out the help of a qualified provider to assist you in diagnosing and treating pelvic organ prolapse and any other pelvic floor dysfunction, which brings me to my first point.
1. Seek out the guidance of a pelvic floor physical therapist.
If you are dealing with pelvic organ prolapse and are concerned about how it will impact your pregnancy, the first step is seeking out the guidance of a pelvic floor physical therapist. They can help you with an individualized treatment plan and give you more guided advice regarding regarding birth. I fully recognize that not everyone has the ability to seek out therapy, whether it be for time, distance, or financial reasons. If you don’t have a PFPT in your area, many do remote sessions which can be tremendously helpful. If you can’t seek out treatment for financial reasons, even going for a consultation can be so helpful for you. Managing POP is about finding a team of support people who will help you reach your individual goals in an understanding, empathetic, and open-minded way. Which brings me right to my next point...
You can find a pelvic floor physical therapist in your area using the directory at pelvicguru.com
2. If you are active or want to remain active, seek out the help of a coach who is trained to work with women who have POP.
Most people think that activity and POP do not go together, but staying active can actually be really good for the pelvic floor and a necessary part of healing. However in some cases it may be more difficult to find an activity that works for you without increasing symptoms. This is where a well-trained professional comes in handy.
If you are active going into pregnancy or wanting to start an exercise routine in pregnancy, but are fearful of making pelvic floor symptoms worse- a coach trained in working with pregnant women with POP can be such a valuable resource. We can help you by designing a program appropriate for your body, keeping tabs on your symptoms and suggesting modifications, and scale your exercise according to stage of pregnancy and goals. Not only that, but we can also assist you in returning to exercise after birth
You can also find a coach near you using the directory above. Many of us also work remotely, so please don’t hesitate to reach out using the “contact me” tab!
3. Know that symptoms may ebb and flow.
Pregnancy is a time full of huge hormone fluctuations as well as physical changes. This likely means that there are times where your symptoms may be worse than others. It is really common for clients of mine to stress out about what they may have done to make their symptoms worse. And here’s what I often tell them:
“It probably isn’t anything you did or didn’t do.”
This is especially true during times where hormones shift, like pregnancy, ovulation, during your menstrual cycle, or around menopause. Changes in symptoms could also happen as your belly begins to get bigger.
Here are 3 things you can do when you notice symptoms flaring:
Take note of your stress/sleep levels. Are you particularly stressed? Sleep been all out of whack? Sudden onset of morning sickness? These events can trigger an increase in symptoms. Take a breath and focus a bit more on self-care when you can.
Add in pelvic floor releasing/strengthening exercises to your day. When you notice symptoms are worse during the day, take a few minutes to do a few pelvic floor relaxation AND strengthening exercises. This can help manage symptoms and also take care of #1.
Continue to stay active. Often an increase in symptoms can come with a fear of activity, but so often continuing to be active in a way that doesn’t increase symptoms can help both mentally and physically. Continue to exercise or stay moving in a way that feels good for you. Prioritizing longer rest periods and/or using lower loads and intensity can help manage symptoms that have flared.
How Does Birth Affect Pelvic Organ Prolapse?
This is a question a lot of women ask and there’s so much to cover that I’m going to write a separate article on this subject. However, I do want to touch on it here.
Ultimately HOW you birth is up to you. A lot of research suggests that the most trauma to the pelvic floor happens during the first birthing experience (more on this in the next article.) Whether you can control more damage to the pelvic floor by choosing a C-section over a vaginal birth is a very big topic, one in which research is lacking on. Here are the things that matter:
YOU feel comfortable and calm about your birthing decision
Whatever you choose helps manage your anxieties and supports you emotionally during birth/postpartum
You have the proper support no matter how you choose to birth
You have the ability to choose positions that you feel comfortable laboring/pushing in during birth
I’ll go into more detail on these in a subsequent article because I want this to be a starting point for you- not too overwhelming. But, for now, I want to link to this amazing interview done by my friend Jeanice at MyPFM on birth positions avoiding orthopedic injury that you may find super helpful!
Conclusion
If you are managing POP during pregnancy, know that you aren’t alone. The most important thing is to surround yourself with a positive support team who cares about your experience and your goals. If you’re nearing or in your third trimester and need help navigating exercise in a way that feels safe for your body and also preparing for birth, my inbox is always open- I’d love to chat about how I may be able to help you.